Study design and participant characteristics
The study population consisted of children and adolescents from the HOLBAEK study, previously known as the Danish Childhood Obesity Biobank14,15, including an obesity clinic cohort, in which children and adolescents with a BMI ≥ 90th percentile (BMI standard deviation score (SDS) ≥ 1.28) according to a Danish ref. 23 participated in a multidisciplinary nonpharmacological obesity management program at the Children’s Obesity Clinic, Holbæk Hospital; and a population-based cohort, recruited from schools across 11 municipalities in Zealand, Denmark.
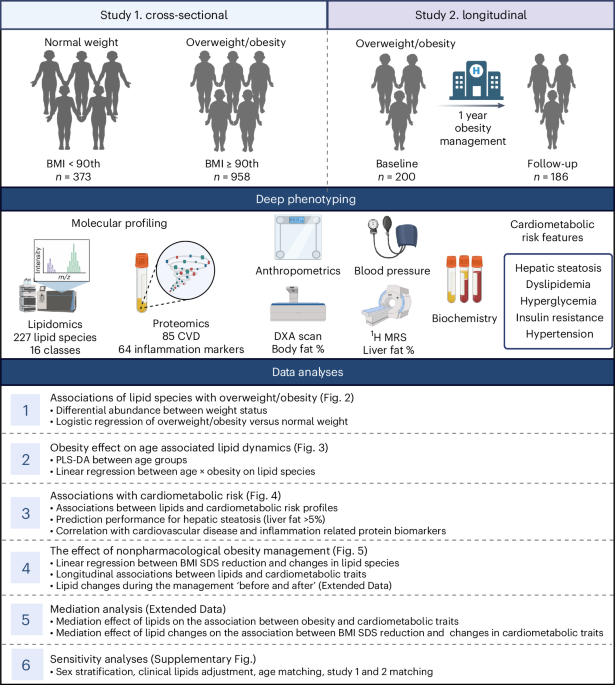
Anthropometry, whole-body dual-energy X-ray absorptiometry (DXA) scan24, proton magnetic resonance spectroscopy (1H-MRS)25 and blood parameters26,27,28,29,30,31,32 were assessed as described previously. Untargeted lipidomic profiling was performed on 1,363 children and adolescents who had baseline examinations, as well as 186 participants who received obesity management at baseline and had a median follow-up duration of 1.1 years. We performed a cross-sectional analysis on 1,331 participants divided into normal weight (n = 373) and overweight/obesity groups (n = 958) and a longitudinal analysis on 186 children and adolescents with overweight or obesity. A schematic study design is shown in Fig. 1.
Lipidomic profiles were measured in 373 children and adolescents with normal weight and 958 with overweight or obesity. We investigated lipid dysregulation in relation to overweight/obesity, cardiometabolic risk profiles, known CVD-related and inflammatory markers, and the predictive ability to detect hepatic steatosis. In addition, lipidomic profiles were measured in a subset of children and adolescents who received nonpharmacological obesity treatment. The lipidome response to BMI SDS reduction and longitudinal associations between lipids and cardiometabolic traits were examined. Mediation and sensitivity analyses were conducted. Created with BioRender.com.
In the cross-sectional study, the overweight/obesity and normal weight groups differed significantly in anthropometrics and cardiometabolic risk profiles except for sex, lactate dehydrogenase (LDH) and hemoglobin A1c (HbA1c). Specifically, the overweight/obesity group had higher BMI SDS, waist, waist/hip ratio (WHR), body fat %, liver fat % and elevated levels of liver enzymes such as alanine transaminase (ALT), aspartate transaminase (AST) and γ-glutamyl transferase (GGT). They also exhibited elevated levels of traditional lipids, including low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC) and TG, as well as higher glycemic parameters, including glucose, insulin, C-peptide and homeostasis model assessment of insulin resistance (HOMA-IR). Other notable differences included higher high-sensitivity C-reactive protein (hs-CRP), leptin, leptin/adiponectin ratio, glucagon, total glucagon-like peptide-1 (GLP-1), systolic blood pressure (SBP) SDS and diastolic blood pressure (DBP) SDS. They also had lower levels of high-density lipoprotein cholesterol (HDL-C) and adiponectin (Table 1). In comparison to the normal weight group, the overweight/obesity group exhibited a higher prevalence of hepatic steatosis defined as liver fat ≥ 5.0 % (15.6% versus 0%), high ALT (38.7% versus 12.6%), dyslipidemia (38.0% versus 10.8%), hyperglycemia (14.0% versus 8.6%), insulin resistance (35.0% versus 5.6%) and hypertension (15.9% versus 3.0%) (all P < 0.05).
Associations of lipid species with overweight or obesity
Differentially abundant lipids revealed a gradual change among the three weight statuses (normal weight, overweight and obesity), after adjusting for age and sex. Among 227 annotated lipid species, 142 exhibited significant differences across normal weight, overweight and obesity (P < 5% false discovery rate (FDR)). The pairwise comparisons revealed 121 lipids significantly differed between normal weight and obesity, 43 between overweight and normal weight and 60 between overweight and obesity (Fig. 2a).

a, Significant differences were identified in the mean normalized intensities of 142 lipid species across normal weight, overweight and obesity (n = 373, 192 and 766, respectively). Analysis was performed using an analysis of variance (ANOVA), with P values adjusted for multiple testing using the FDR method (P < 5% FDR). Three paired comparisons were subsequently conducted using Tukey’s HSD test. b, Overall, 87 lipid species were associated with overweight/obesity compared to normal weight tested by logistic regression adjusted for age and sex (n = 958 and 373, P < 5% FDR). Bubble plot showing the odds ratio (OR) with error bars representing the 95% CI of lipid species in each lipid class. Gray circles denote nonsignificant associations. The proportion of significant associations (P < 5% FDR, orange denotes positive and blue denotes negative) in each lipid class are shown.
Logistic regression analyses for normal weight versus overweight/obesity revealed 87 significant lipid species in 13 lipid classes, of which 52 were positively and 35 were negatively associated, independent of age and sex (P < 5% FDR). Notably, 20% measured Cers (3 of 15), 33% measured SMs (5 of 15), 47% TGs (25 of 53), all diacylglyceride (DG) (2 of 2) and 40% FAs (2 of 5) were positively associated, whereas the majority of glycerophospholipids, including 33% N,N-dimethyl-phosphatidylethanolamine (dMePE) (1 of 3), 30% lysophosphatidylcholine (LPC) (7 of 23) and 60% lysophosphatidyethanolamine (LPE) (3 of 5) displayed negative associations and PCs, PEs and PIs showed more divergent trends in associations: 14% and 20% PCs (9 and 13 of 64), 25% and 17% PEs (3 and 2 of 12) and 12% and 38% PIs (1 and 3 of 8) had significant positive and negative associations (Fig. 2b, Extended Data Fig. 1 and Supplementary Table 1).
The interaction of obesity with age related lipid species
A partial least squares-discriminant analysis (PLS-DA) score plot of lipids between three age groups in normal weight and overweight/obesity groups is shown in Fig. 3a,b. Three age groups (age group 1, girls aged <9 years and boys aged <10 years; age group 2, girls aged 9–15 years and boys aged 10–16 years; age group 3, girls aged >15 years and boys aged >16 years) were defined according to the approximate pubertal development33. Compared to the more pronounced separation between age groups 1 and 2 (larger than between age groups 2 and 3) in the normal weight group, age group 1 did not yield such a clear separation in the overweight/obesity group. We, therefore, assessed whether weight status modifies the association between continuous age and lipid species by including an interaction term ((overweight/obesity versus normal weight) × age) for each lipid species, adjusting for sex. Significant interactions (P < 0.05) were detected in 26 lipid species, with lysophospholipids showing the most pronounced increase with age in the normal weight group compared to the overweight/obesity group, including lysodimethylphosphatidylethanolamine (LdMePE) (0:0 and 16:0) (β = 0.40 in normal weight versus β = 0.23 in overweight/obesity, P = 0.005), LdMePE (16:0 and 0:0) (β = 0.33 versus β = 0.19, P = 0.016), LPC (0:0 and 16:0) (β = 0.39 versus β = 0.24, P = 0.007), LPC (16:0 and 0:0) (β = 0.38 versus β = 0.20, P = 0.001) (Fig. 3c, Extended Data Fig. 2 and Supplementary Table 2). Two polyunsaturated FAs, FA(20:4) and FA(22:6), were decreased with age only in the overweight/obesity group. We detected statistically significant lower levels of these five lysophospholipids in age group 3 when comparing participants with normal weight to participants with overweight or obesity (Fig. 3d).

a, PLS-DA score plot of lipid species in children with normal weight between three age groups. b, PLS-DA score plot of lipid species in children with overweight or obesity from three age groups. c, Associations between age and 26 lipid species that showed significant obesity (overweight/obesity versus normal weight) interaction (P < 0.05). Linear regression analysis was performed including an interaction term for obesity and adjusting for sex. The β-coefficients with error bars representing 95% CI were shown separately for the normal weight (green) and overweight/obesity group (red). n = 958 and 373 for overweight/obesity versus normal weight. d, Box plot showed the normalized intensities of five lysophospholipids that were most increased in normal weight children among three age groups. Data are presented as median values, box edges are IQR (25th to 75th percentiles) and whiskers represent 1.5 × IQR. An asterisk indicates a significant difference between two groups (P < 0.05). NS, not significant. n = 207, 126 and 40 and 212, 612 and 134 for age group 1, 2 and 3 in the normal weight and overweight/obesity group, respectively.
Considering the age gap between the overweight/obesity and normal weight groups, we matched individuals in the obesity group to the normal weight group by age and sex. The subanalysis confirmed a significant obesity interaction on lysophospholipids (Supplementary Fig. 1).
Associations of lipid species with cardiometabolic risk
A total of 135 lipids had at least one significant association (P < 5% FDR) with cardiometabolic risk feature after adjusting for age, sex and BMI SDS (Extended Data Fig. 3a and Supplementary Table 3). Seventeen sphingolipids, including 9 Cers, were associated with higher prevalence of hepatic steatosis, dyslipidemia and insulin resistance, whereas 8 SMs were associated with lower prevalence. Nine PEs and eight PIs were shown to have positive associations with hepatic steatosis, dyslipidemia and insulin resistance (Fig. 4a).

a, The 34 lipids including Cer, SM, PE and PI species having at least one significant association with one cardiometabolic risk feature (P < 5% FDR). Logistic regression analysis was performed adjusting for age, sex and BMI SDS. Their associations with cardiometabolic traits tested by linear regression are shown in parallel. b, The discriminant accuracy of three lipids and liver enzymes for diagnosing hepatic steatosis, defined as liver fat ≥5.0%. The analysis includes data from 479 participants, among whom 71 cases of hepatic steatosis were identified. Each curve is accompanied by its corresponding 95% CI, depicted as a shaded area. The mean AUC values with their respective 95% CI are also provided for each ROC curve. c, Correlations of these cardiometabolic-associated lipid species with CVD and inflammation (INF)-related protein biomarkers were calculated using two-sided Spearman correlation. The size of the link represents the number of significant correlations (Spearman r > 0.2 and P < 5% FDR). Nine sphingolipids correlated with ten CVD markers, one sphingolipid correlated with one INF marker. Ten PEs and PIs correlated with 15 CVD markers and six PEs and PIs correlated with six INF markers. d, Two-sided Spearman correlations are shown. *P < 5% FDR; #P < 2.2 × 10−4. The sample size (n) for each feature/trait is listed in Table 1; the maximum observed is 1,330.
In total, 207 lipids had at least one significant association (P < 5% FDR) with cardiometabolic trait after adjusting for age, sex and BMI SDS (Extended Data Fig. 3b and Supplementary Table 4). We explored potential sex differences in the associations between lipid species and cardiometabolic traits, identifying 13 lipid species that demonstrated significant sex interactions (P < 5% FDR) with eight cardiometabolic traits (Supplementary Fig. 2). Sex-specific effect estimates are provided in Supplementary Table 5.
The associations between the 34 cardiometabolic risk feature-associated Cers, SMs, PEs and PIs with continuous cardiometabolic traits are shown (Fig. 4a). Specific Cers were positively associated with liver-related traits (liver fat %, ALT, AST and GGT), traditional lipids (LDL-C, TC and TG) and glycemic traits (C-peptide, HOMA-IR, insulin and glucose), glucagon and GLP-1, but not with hs-CRP or blood pressure. SMs showed negative associations with TG, liver and glycemic traits, leptin:adiponectin ratio and GLP-1. Furthermore, PIs and PEs were positively associated with liver and glycemic traits, leptin:adiponectin ratio and GLP-1. PIs were also linked to higher levels of hs-CRP, glucagon and DBP SDS. In a sensitivity analysis, further adjustment for TC and TG attenuated certain associations between lipids and liver and glycemic traits; however, the majority of distinct associations persisted (Supplementary Fig. 3)
We further tested the effect of weight status on the associations between the above-mentioned 34 Cers, SMs, PEs and PIs with cardiometabolic traits, adjusting for age and sex. Significant interactions were detected between 25 lipids with 14 traits (P < 5% FDR) (Extended Data Fig. 4 and Supplementary Table 6). In particular, significant associations were observed between Cers, SMs, PEs and PIs with ALT and GGT, SMs with insulin and PIs with hs-CRP, leptin, glucagon, GLP-1 and DBP SDS; a larger effect size in children and adolescents with overweight or obesity compared to participants with normal weight.
Predictive performance of lipids to detect hepatic steatosis
Given their clinical relevance, we explored the predictive potential of cardiometabolic-associated lipids for detecting hepatic steatosis, defined as liver fat above 5%. Employing feature selection techniques, we identified a three-lipid panel comprising PI(32:1), PE(36:1) and Cer(d42:0). This panel demonstrated a mean cross-validated receiver operating characteristic (ROC) area under the curve (AUC) of 0.79 (95% CI 0.77–0.81) through fivefold cross-validation repeated ten times (Fig. 4b). Furthermore, integration of this lipid panel with three liver enzymes (ALT, AST and GGT) significantly increased the AUC from 0.78 (95% CI 0.76–0.8) to 0.82 (95% CI 0.81–0.84) (as determined by DeLong’s test, P < 0.05).
Correlations of lipids with CVD and inflammatory markers
Correlation between the 34 cardiometabolic-associated Cers, SMs, PEs and PIs with markers from CVD and INF panels revealed significant correlations between nine sphingolipids and ten CVD markers and Cer(d42:0) with inflammatory marker CDCP1. Additionally, 10 PEs and PIs correlated with 15 CVD markers and 6 PEs and PIs correlated with 6 inflammatory markers (Spearman correlation r > 0.2 and P < 5% FDR) (Fig. 4c and Supplementary Table 7). Positive correlations were detected between Cers, PEs and PIs with CVD markers, including FGF21, PRSS8, SPON2, HAOX1, LEP and ADM, whereas SMs were negatively correlated. PEs and PIs also correlated with inflammatory markers, including VEGFA, IL-18R1 and HGF, among others (Fig. 4d).
Mediation effect of lipids on cardiometabolic traits
We conducted mediation analysis to explore the role of 87 obesity-associated lipids on cardiometabolic traits, adjusting for age and sex. Overall, 83 lipids significantly mediated the effect of obesity on 19 cardiometabolic traits, with a median mediation proportion of 5% (Extended Data Fig. 5 and Supplementary Table 8). Notably, certain PCs and TGs exhibited particularly substantial mediation proportions, surpassing 20% in traditional lipid profiles. Specifically, TG(52:1) demonstrated partial mediation effects across cardiometabolic traits. Additionally, SMs, LPEs and LPCs were found to exert a negative mediation effect on the association between obesity and glycemic traits, with mediation proportions ranging from 5% to 23% for glucose.
The effect of personalized obesity management
A subset of 186 children and adolescents with overweight or obesity, comprising 84 boys and with a median age of 11.6 years (interquartile range (IQR) 9.9–13.7), underwent obesity management for a median duration of 1.1 years (IQR 1.0–1.2). Among them, 154 participants experienced a decrease in BMI SDS, whereas 32 maintained or increased their BMI SDS. Across all participants, there was a median reduction in BMI SDS of −0.39 (IQR −0.76 to −0.07) from baseline to follow-up, accompanied by a median decrease in body fat content of −2.85 (IQR −6.53 to −0.38) (P < 0.001). Furthermore, significant improvements were observed in WHR, LDH, TC, HDL-C, LDL-C, HbA1c and DBP SDS (all P < 0.001) (Extended Data Table 1). Liver enzymes (ALT, AST, GGT and bilirubin) and glycemic traits (C-peptide, insulin and glucose) did not show significant improvements in all participants or the subgroup with decreased BMI SDS, but worsened in those who increased BMI SDS.
Before investigating the lipidome response to obesity management, we examined the baseline associations of BMI SDS with lipids and how these associations evolved with BMI SDS reduction. Utilizing the baseline data from the intervention study as a replication set, we found that 25 of 58 lipids associated with BMI SDS in children with overweight/obesity from the cross-sectional study (P < 5% FDR, n = 958) also exhibited significant and consistent associations at baseline in the intervention study (P < 5% FDR, n = 186). Additionally, 24 lipids showed directionally consistent trends but did not reach statistical significance (Supplementary Fig. 4).
A comparison of lipid profiles before and after obesity management revealed significant changes. Among the 145 lipids examined, significant increases were observed in 44 lipids, including PCs, LPCs and LPEs (P < 5% FDR). In contrast, 23 lipids, including Cers, SM and TGs were significantly decreased (Extended Data Fig. 6 and Supplementary Table 9).
Furthermore, we investigated the lipidome changes in response to continuous BMI SDS reduction and their associations with cardiometabolic traits. A total of 62 lipid species demonstrated significant associations with BMI SDS reduction, out of which 45 were also significantly associated with BMI SDS at baseline (P < 5% FDR). Of note, TGs exhibited the greatest reduction following BMI SDS reduction. Additionally, nine sphingolipids including Cers and SMs and four glycerophospholipids, including PEs and PIs were significantly decreased (Fig. 5a, Extended Data Fig. 7 and Supplementary Table 10).

a, BMI SDS reduction was associated with changes in 62 lipids tested by linear regression, adjusting for age, sex and treatment duration (n = 186, P < 5% FDR). The β-coefficients with error bars representing 95% CI are shown. b, Changes in Cers, SMs, PEs and PIs were associated with changes in cardiometabolic traits tested by linear regression, adjusting for age, sex, treatment duration, baseline BMI SDS and change in BMI SDS (P < 5% FDR). BMI SDS reduction was calculated as the difference between BMI SDS at baseline and BMI SDS at follow-up. Changes in lipid profiles and cardiometabolic traits were calculated as the difference between the values at follow-up and those at baseline. +P < 0.05; *P < 5% FDR. c, Alluvial plot to illustrate the overall lipid class inter cohort validation, response to weight loss and proportion of mediation links: 25 validated lipids in seven lipid classes associated with baseline BMI SDS using data from overweight/obesity group in the cross-sectional (n = 958) and baseline data from children with obesity (n = 186) in the intervention study (left). Twenty-two of these lipids in six classes were significantly (P < 5% FDR) decreased with BMI SDS reduction (middle). The significant mediator role of changes in these lipids in the association between changes in BMI SDS and changes in cardiometabolic traits (right, n = 21). The colors of curved lines represent different lipid classes. NA indicates that three lipids, which did not significantly change with BMI SDS reduction, were not applicable for mediation effect. NS, nonsignificant indirect effect from mediation analysis. The sample size (n) for each trait is listed in Supplementary Table 9; the maximum observed is 185.
Longitudinal analyses revealed associations between changes in Cers, SMs, PEs and PIs families with changes in cardiometabolic traits that were independent of age, sex, treatment duration, baseline BMI SDS and change in BMI SDS at nominal significance (P < 0.05) (Fig. 5b, Extended Data Fig. 8 and Supplementary Table 11). Changes in these cardiometabolic-associated lipid profiles were significantly associated with changes in traditional lipids. Changes in Cer(d42:0) and Cer(d42:1) were positively associated with changes in ALT at a nominal significance level. Changes in SM(d36:1) and SM(d36:2) were associated with changes in bilirubin and negatively associated with changes in HOMA-IR and glucose. Longitudinal positive associations were observed between certain PEs and PIs with ALT, HOMA-IR and glucose.
Mediation effect of lipid changes on cardiometabolic traits
We investigated whether changes in lipid species potentially mediate the relationship between reductions in BMI SDS and changes in cardiometabolic traits. A reduction in BMI SDS was associated with changes in 11 cardiometabolic traits and changes in 70 lipids. Out of 253 tested paths, 216 paths exhibited a significant indirect effect, with a median proportion of 23% (Extended Data Fig. 9 and Supplementary Table 12). Changes in 65 lipids significantly mediated the association of BMI SDS reduction and changes in traditional lipids, with mediation proportions ranging from 7% to 60%. Furthermore, changes in Cer(d42:0) mediated an 18% reduction in ALT, while some PCs and TGs mediated improvements in HOMA-IR and insulin levels, with proportions ranging from 9% to 26%.
To consolidate the intervention results a subset of lipids (n = 25) from seven lipid classes replicated with baseline BMI SDS using data from overweight/obesity group in the cross-sectional and baseline data from children with obesity in the intervention study were selected. Twenty-two of these lipids in six lipid classes were significantly (P < 5% FDR) decreased with BMI SDS reduction. Of these, 21 lipids mediated changes in cardiometabolic traits (Fig. 5c and Supplementary Table 13).