In this study, we attempted to find an association between the serum aldosterone levels measured on days 1, 3, 5, and 7 and the overall survival in the intensive care unit (ICU) for a duration of 28Â days. Even though the mean plasma aldosterone levels were higher in the patients who did not survive for 28Â days, the results were not statistically significant, indicating that aldosterone is not associated with ICU mortality. A previous study by Villard et al.14 reported a worse disease course in patients with higher aldosterone levels at admission; specifically, those with higher plasma aldosterone levels were more likely to be admitted to the ICU. This might indicate that plasma aldosterone levels might be associated with the rate of admissions to ICUs but do not correlate with overall days survived in the ICU. Studies suggest that SARS-CoV-2, by competing with angiotensin II for the ACE2 receptor, indirectly increases Ang-II levels, which should increase aldosterone biosynthesis. It is possible that aldosterone production in COVID-19 patients increases with disease severity and reaches a peak when the state of the patient calls for an ICU admission. More research is needed to reach a definite conclusion.
Systemic inflammation evoked by SARS-CoV-2 is a hallmark of COVID-19, and one of the most widely used biomarkers for inflammation is an acute-phase protein CRP, which is biosynthesized in the liver in response to elevated interleukin-6 levels14,15. Interestingly, our results showed statistically significantly lower levels of serum CRP in patients who died during their 28-day stay in the ICU, yet it was not associated with higher mortality. This outcome contradicts previous findings indicating a relationship between CRP serum concentration and severity of the disease16,17,18,19,20. This discrepancy could be a result of the small size of the group that survived beyond 28Â days.
Higher serum creatinine levels have been shown to be another strong predictor of ICU admission and mortality21. Our study provides additional evidence that high serum creatinine concentration is a predictor of COVID-related ICU mortality; higher creatinine levels were observed on days 1, 3, and 5 in patients who died within 28Â days than in the group of individuals who survived. Many large studies, including meta-analyses, have confirmed the association of high creatinine levels with increased mortality in severely ill patients21,22,23.
In our study, univariate analysis showed increased mortality in the group of patients with higher APACHE II, SAPS II, and SOFA scores. Multivariate analysis showed that age (HRâ=â1.03, pâ=â0.033) was a robust predictor of mortality in the entire study population, similar to the finding of the meta-analysis by Kowsar et al.24. COVID-19 is a disease with a difficult-to-predict course. In intensive care units, numerous scales are routinely used to assess the risk of death and estimate the severity of the condition and organ function upon admission. Our study selected the most frequently used and valuable ICU scales. In a study by Monk et al., no advantage of any mortality scoring systems applied to COVID-19 was demonstrated. The study showed that SOFA, SAPS II, APACHE II, and ISARIC 4-C scores accurately predicted mortality in critically ill patients with COVID-19. The SOFA score executed the best. The study conducted by our team showed correlations of the values obtained in the SOFA, APACHE II, and SAPS II scales with mortality12.
Comorbidities associated with higher mortality following SARS-CoV-2 infection are hypertension and diabetes. There is a strong association between in-hospital mortality due to COVID-19 and hypertension, coronary heart disease, and diabetes25, although our study did not show a statistically significant effect of these factors on mortality. Researchers have postulated that the use of RAS blockers, such as ACE inhibitors or angiotensin receptor blockers (ARB), which are frequently administered in these conditions, might contribute to upregulation of ACE2, which could potentially promote cell entry of SARS-CoV-2, causing worse outcomes. The BRACE CORONA clinical trial later proved that neither continuation nor discontinuation of these drugs had a significant impact on mortality or COVID-19 progression26. Mineralocorticoid antagonists have also failed to show any effect on mortality in a recent meta-analysis27. The activation of RAAS by SARS-CoV-2 may lead to a direct increase in aldosterone production; one of the production sites may be the endothelial cells of the pulmonary vessels29. Higher levels of aldosterone may induce severe forms of COVID-19, especially in older patients, by promoting the inflammatory response and inducing electrolyte disorders such as hypokalemia.
One of the treatment options for COVID-19, in the case of high aldosterone concentration correlation with mortality, could be the use of mineralocorticosteroid receptor antagonists (MRAs). Reports on the effect of MRAs on COVID-19 are ambiguous22,28,29. MRAs, ACE inhibitors (ACE-I), and angiotensin receptor blockers (ARBs) were analyzed for their effects on COVID-19. Many patients discontinued RAASi treatment during the first phase of the COVID-19 pandemic due to the potential for these drugs to increase ACE 2 expression and levels. Numerous studies have shown that RAASi use is not linked to the risk of COVID-1928,29,30. Compared to ACE-I and ARBs, using MRAs in COVID-19 may provide some benefits. Additionally, MRAs, by stimulating ADAM metalloproteinase domain 17 protein, increases circulating ACE 2, which might bind SARS-CoV-2 as a competitive interceptor29. MRAs can suppress the expression of type II transmembrane serine protease TMPRSS2, which increases viral uptake of SARS-CoV-2 in target cells by promoting membrane fusion of Spike glycoprotein through a proteolytic cleavage between the S1 and S2 subunits and, also, by cleaving ACE 2 that, in turn, activates cathepsin L-dependent pathway31.
Inhibiting these pathways induced by MRAs could suppress or reduce viral entry in human cells. It might benefit COVID-19 infection and acute respiratory distress syndrome32,33. The reason why aldosterone levels were measured in our ward was to investigate the correlation of its level with mortality, which could potentially result in appropriate treatment. The result of our study did not justify the rationale for use of MRAs in the treatment of Covid-19 patients.
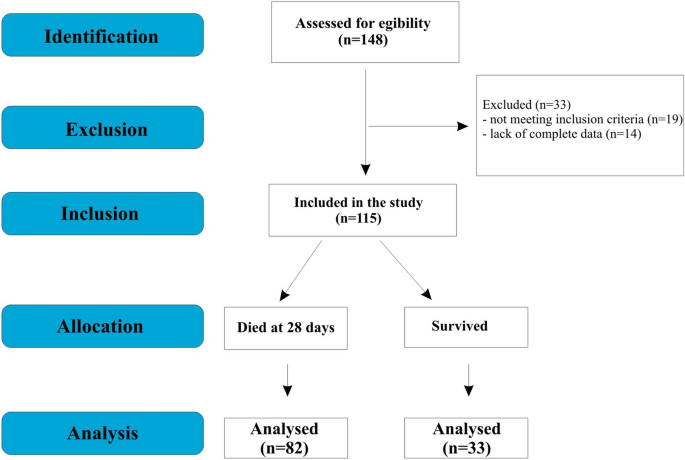
This study has certain limitations that need to be considered when interpreting the findings. First, this is a single-center study with a small simple size. Second, it is a retrospective, cross-selection study; thus, further prospective studies should verify the findings. Further, the chemiluminescent immunoassay method may not reveal aldosterone serum levels. Wiegand et al.34 demonstrated that âaldosterone cannot be accurately estimated in serum from patients with SARS-CoV-2 infection using direct competitive immunoassay. When measured using gold-standard LCMSMS, serum aldosterone is found to be remarkably low in most patients with COVID-19â. However, the chemiluminescent immunoassay method used for aldosterone determination in our study is a well-validated measurement method that is routinely used for aldosterone level determinations in laboratory practice. The method used in the study was compared with a manual radioimmunoassay (RIA), in accordance with the guidelines of CLSI EP9 (Clinical & Laboratory Standards InstituteâMeasurement Procedure Comparison and Bias Estimation). The correlation coefficients were 0.98 (for serum) and 0.90 (for urine). In addition, this parameter is subject to monthly international control (RIQAS external quality control system run by Randox).