Pharmacophore modeling and validation
Five features pharmacophore model (Fig. 3) was generated by applying partial match search on (at least four features) a training set of 12 dual hIDO1/hTDO2 inhibitors. The five features of the model are F1:Aro|Hyd (Radiusâ=â1.5 à ), F2:Aro|Hyd (Radiusâ=â1.5 à ), F3:Aro|Hyd (Radiusâ=â0.7 à ), F4:ML|Acc|Don (Radiusâ=â1.3 à ) and F5:ML&(Acc|Don) (Radiusâ=â0.4 à ); where Aro|Hyd is the aromatic or hydrophobic center, Acc. is H-bond acceptor and Don is H-bond donor. Only four of them are essential whereas F4:ML|Acc|Don is the non-essential feature.
Ligand-based pharmacophore model features.
For the two-dimensional properties of the features, the centroid of F1 created an angle of 44.8° with F3 and F4 with distances equal to 4.85 à and 3.67 à , respectively. F2 centroid showed an angle of 62.7° between F4 and F5 with distances of 4.13 à and 4.37 à , respectively. Moreover, F3 lies between F1, as mentioned earlier, and F5, whose centroid is 1.04 à away from F3 centroid with an angle of 124.5°. In addition, F4 is located between F1 and F2, as mentioned earlier, with an angle of 124.4°. Finally, F5 is located between F2 and F3 with an angle of 64.7°.
On the other hand, to describe the pharmacophore model in a three-dimensional mode, the pharmacophore XYZ coordinates for each feature was determined: (F1: (0.6502, 2.0583, 2.4823), F2: (â 4.1278, â 0.8281, â 1.5894), F3: (â 0.6952, â 2.0007, 0.1855), F4: (â 0.636, 1.2624, â 0.8650), and F5: (â 0.9913, â 2.8787, 0.6632).
For model validation, internal validation of the training set was performed resulting in identifying all the hits 12 used for building the pharmacophoric model (Table 1). Seven compounds out of the 12 fit all the five pharmacophoric features while 5 compounds fit the four essential features.
Additionally, two types of external validations were conducted to extensively test the model validity before its deployment in the virtual screening process. Initially, a test set of 56 active compounds was used to validate the designed model (compound structures are not shown). This was followed by testing the model with a 207 decoys test set. In both cases the model demonstrated efficiency and reliability. 45 true positives out of 56 active compounds were obtained while only 16 false positives out of 207 decoys were identified. Overall, the model demonstrated a high accuracy of 89.73%, a sensitivity (TPR) of 80.36%, a specificity of 92.27%, a False Positive Rate (FPR) of 7.73%, a positive predictive value of 73.77%, and a negative predictive value of 94.55%.
Pharmacophore filtration of FDA-approved drugs dataset
Applying pharmacophore search on a dataset of 2568 FDA-approved drugs has resulted in identifying 958 candidates fitting the designed pharmacophore model features. After a second round of filtration through applying Lipinskiâs and Veberâs rules of drug-likeness, the number of candidates declined to only 308 candidates. The top 10 FDA-approved drugs were found to be fitting all five or at least the four essential pharmacophore features and are listed in Table 2.
Docking validation and high throughput virtual screening
The co-crystal structures of hIDO1 in complex with 1-(4-cyanophenyl)-3-[[3-(2-cyclopropylethynyl)imidazo[2,1-b][1,3]thiazol-5-yl]methyl]urea (PDB ID: 6KPS) and hTDO2 in complex with (3S)-3-(5-fluoro-1H-indol-3-yl)pyrrolidine-2,5-dione (PDB ID: 6PYY) were obtained from the Protein Data Bank. hIDO1 is a monomer α-helical protein comprising 403 residues and a heme prosthetic group. The large C-terminal domain containing the active site consists of 13 α helices and two 310 helices while the small N-terminal domain contains six-α helices, two short β-sheets, and three 310 helices22.
On the other hand, hTDO2 is a homotetramer consisting of 406 residues (15 α-helices without β-strands) and a heme prosthetic group per monomer23.
To validate the docking protocol, self-docking of the co-crystallized ligand was performed. The co-crystallized ligands showed poses and interactions identical to the reported ones; RMSDâ=â1.5325 and 0.3952 à , S-scoresâ=ââ 7.96 and â 7.07 kcal/mol, for hIDO1 and hTDO2, respectively.
A virtual screening study was performed on a dataset of 308 FDA-approved drugs; obtained from pharmacophore search and filtration based on Lipinskiâs and Veberâs rules, against both hIDO1 and hTDO2 proteins. Regarding hIDO1, the virtual screening results showed that 17 FDA-approved drugs out of 308 drugs were found to have higher S-scores than that of the co-crystallized ligand of PDB ID 6KPS (Sâ=ââ 7.96 kcal/mol). While in hTDO2 screening, 126 drugs out of 308 drugs reported S-scores better than that of the co-crystallized ligand of PDB ID 6PYY (Sâ=ââ 7.07 kcal/mol). Therefore, sequential exclusion criteria were implemented for the top 10 compounds based on the formation of interactions with the heme group and the essential residues for inhibition in IDO1 and TDO2 (Arg231 or Ser167 in hIDO1, Arg144 and His76 in hTDO2), the strength of interactions, addressing potential side effects, S scores, and the commercial availability.
The top ten pharmacophore filtered drugs were found to be amongst the compounds displaying good interactions with both hIDO1 and hTDO2 and eliciting good S scores as shown in Table 3. Yet, only 4 drugs out of the 10 formed interactions with the essential residues needed for the inhibition of both enzymes with high capability of fitting into their active sitesâ pockets (details in the supplementary material Figs. S1 and S2). Therefore, those four drugs, Trovafloxacin, Vilazodone, Pitavastatin and Dasabuvir, were re-docked and their strength of interactions, S scores, potential side effects of each drug, and the commercial availability were scrutinized. Considering the potential side effects of the four drugs, Trovafloxacin was excluded as it is withdrawn from the market. Also, Vilazodone was excluded due to its potential CNS side effects, while Dasabuvir wasnât the one of choice by virtue of its potential side effects as a chemotherapeutic agent as well as its commercial unavailability. Amongst the four, Pitavastatin possesses the safest side effects, and demonstrated essential interactions with the active site amino acids of both target enzymes.
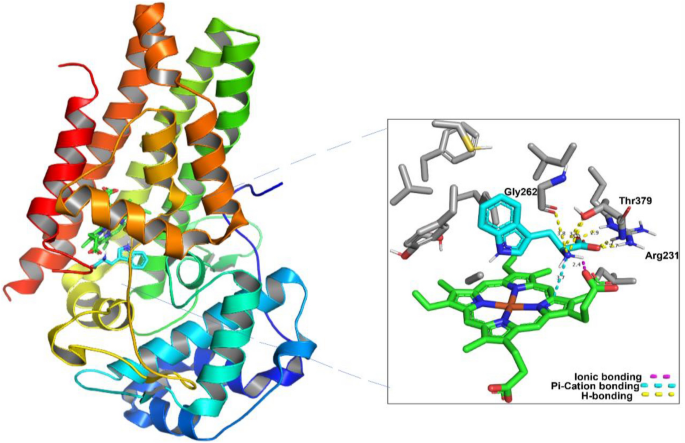
Analyzing Pitavastatin interactions in both enzymes is shown in Fig. 4. Two non-covalent interactions were visualized in hIDO1 (Fig. 4A). The carboxylic moiety in Pitavastatin could form one hydrogen bond acceptor interaction with Arg231 sidechain while the allylic hydroxyl has a Hydrogen bond donor interaction with the C-terminus of Gly262 backbone in hIDO1. This is highly consistent with previous studies that reported the essentiality of inhibiting Arg231 to prevent Trp coordination to the heme, accordingly, blocking Trp catabolism24. Moreover, comparing Fig. 4A to Fig. 1, the interaction with Gly262 indicates the ability of Pitavastatin to occupy pockets A and B of the active site, therefore enhancing the binding affinity to hIDO1 active site.
2D interactions and pocket surface occupancy of Pitavastatin, the best hit shown in Cyan, against hIDO1 (A) and hTDO2 (B). The Heme group is represented in green, the surface map is the Pocket surface occupancy, in which the blue color represents cationic moieties, while red color represents anionic moieties, and the hydrophobic moieties are illustrated in gray.
For hTDO2, as illustrated in Fig. 4B, the quinoline moiety in Pitavastatin formed a ÏâÏ interaction with His76 sidechain. Also, the carboxylic acid moiety in Pitavastatin functioned as a Hydrogen bond acceptor with Arg144 sidechain and the N-terminus of Thr342 backbone while the β-hydroxyl moiety interacted with Thr342 sidechain as a Hydrogen bond donor. Finally, the cyclopropyl moiety could form an H-Arene interaction with the heme group, which is consistent with the pharmacophore fitting highlighting cyclopropyl group as an essential hydrophobic feature. The results are consistent with the previous studies reporting the His76 crucial role as a base catalyst responsible for Trp catabolism, in addition to Arg144âs importance in Trp recognition19. Also, comparing these interactions to those with Trp in Fig. 2, Pitavastatin could fulfill all the essential interactions needed for hTDO2 inhibition. The β-hydroxy acid moiety in Pitavastatin could mimic the interactions of the Trp amino acid moiety with both Thr342 and Arg144. In addition, the presence of quinoline moiety allowed mimicking the Trp indole group interaction as introducing a larger heteroaromatic core enhances the proximity towards His76 and provides larger occupancy into the active site pocket.
Overall, the interacting moieties in Pitavastatin in both enzymes is consistent with its pharmacophore fitting shown in Table 2.
Pitavastatin could pass all the criteria set for identifying a good dual hIDO1/hTDO2 inhibitor as it could fulfill the essential four features of the ligand-based pharmacophore model generated from a set of dual hIDO1/hTDO2 inhibitors as shown in Table 2. In addition to being one of the best scoring hits on both enzymes with best interaction with main reported amino acids in both pockets, Pitavastatin has the safest potential side effects and is commercially available. Moreover, Xu et al.25 has reported its anticancer effect via downregulating AKT and ERK signals. Accordingly, it was elected as the drug of choice for further in vitro evaluation in this study.
Molecular Dynamics simulations
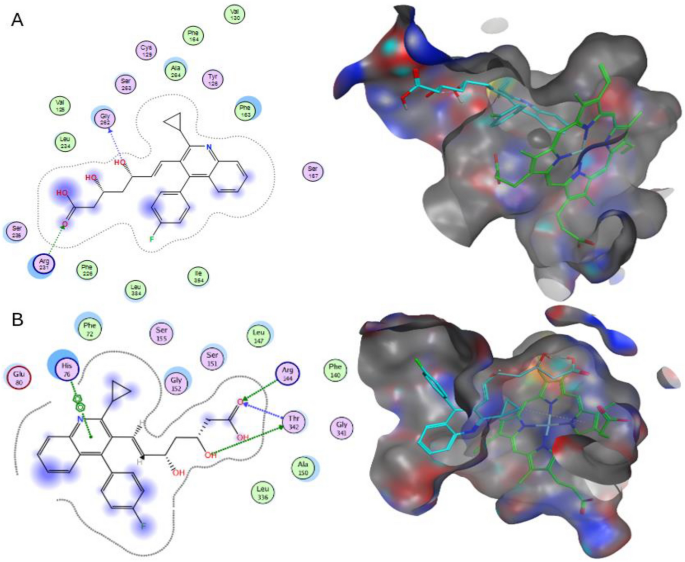
To evaluate the stability of Pitavastatin binding to both target enzymesâ simulated system, we conducted a thorough examination of conformational changes within the proteinâligand complexes using three distinct methodologies: root-mean-square deviation (RMSD), radius of gyration (Rg), and solvent accessible surface area (SASA) analyses for both the ligand and the target throughout the 100 ns of molecular dynamics (MD) simulation (Fig. 5). These parameters were computed subsequent to re-centering and re-wrapping the complexes within the unit cells using the trjconv function within GROMACS.
Structural dynamics of hIDO1 and hTDO2 RMSD upon binding to Pitavastatin and the co-crystalized ligands (A), ligands (Pitavastatin and the co-crystalized ligands) RMSD (B) hIDO1 and hTDO2 radius of gyration (C), SASA values (D) calculated during the 100 ns of MD trajectories.
The RMSD plot, shown in Fig. 5A, provides insight into the stability of the hIDO1 backbone in the presence of both Pitavastatin and its co-crystallized ligand (1-(4-cyanophenyl)-3-[[3-(2-cyclopropylethynyl)imidazo[2,1-b][1,3]thiazol-5-yl]methyl]urea), elucidating conformational changes over the course of the 100 ns MD simulation. Notably, the fluctuation pattern of the hIDO1 backbone in both scenarios closely aligns, demonstrating minimal fluctuation observed for both (depicted in black and red). Similarly, the backbone RMSD of hTDO2 was examined in complex with Pitavastatin and its co-crystallized ligand ((3S)-3-(5-fluoro-1H-indol-3-yl)pyrrolidine-2,5-dione). Binding of Pitavastatin (depicted in blue) resulted in enhanced stability compared to the co-crystallized ligand (depicted in green), with a slightly higher fluctuation observed.
To further validate their relative stability, the ligand RMSD plots upon binding to their respective target receptors (hIDO1 and hTDO2) were generated as referred in Fig. 5B. Remarkably, a notably higher stability was observed upon Pitavastatin binding to the hIDO1 receptor (depicted in red), exhibiting minimal fluctuation compared to the native ligand (depicted in black). For hTDO2, Pitavastatin demonstrated binding to the pocket with relatively high stability approximately after 20 ns from the simulation onset (depicted in blue), oscillating around only 0.1 nm, indicating a very stable interaction.
The compactness of the protein backbone within the four complexes was assessed by visualizing their radius of gyration (Rg) over the entire simulation duration (Fig. 5C). Consistently stable protein backbone compactness was observed for both Pitavastatin and the native ligand upon binding to the hIDO1 receptor (depicted in red and black, respectively). The protein compactness pattern for hTDO2 backbone mirrored the trends observed in the RMSD plot, with high backbone compactness observed following Pitavastatin binding to hTDO2, particularly evident after 20 ns. This stability was further corroborated by SASA plots, demonstrating minimal fluctuation ranging between 200 and 210 nm2 for the two hIDO1 complexes and between 190 and 200 nm2 for hTDO2 complexes throughout the entire simulation duration (Fig. 5D).
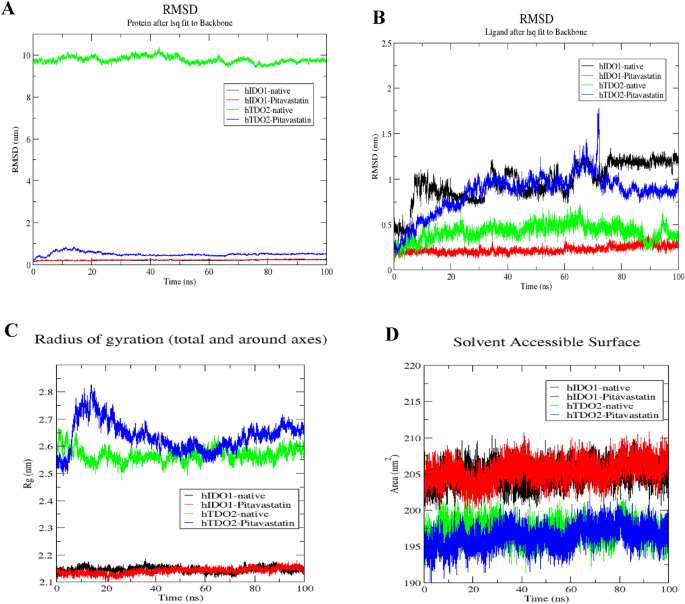
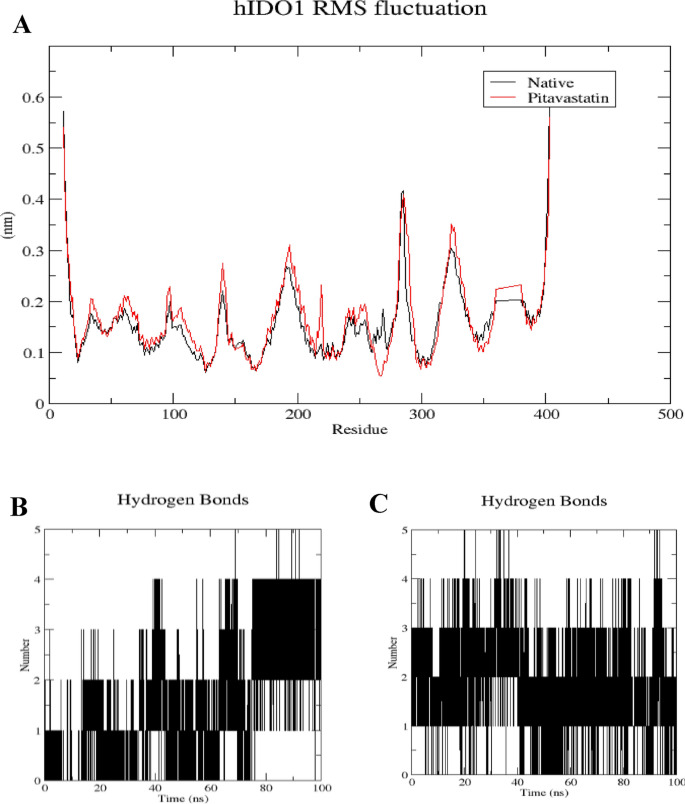
The root mean square fluctuation (RMSF) analysis was conducted to assess the rigidity and flexibility of backbone residues within hIDO1 and hTDO2 throughout the 100 ns of molecular dynamics (MD) simulation. Figures 6A and 7A depict the RMSF patterns for the two hIDO1 complexes and the two hTDO2 complexes, revealing consistent trends across both proteins. Notably, residues involved in ligand interactions exhibited minimal fluctuation, typically less than 0.2 nm, indicative of stable binding interactions. For hIDO1, the two key residues with minimal fluctuations are Gly262 (approximately 0.05 nm) and Arg231 (around 0.1 nm). For hTDO2, the key residues with small fluctuations are His76 (less than 0.2 nm), Arg144(less than 0.15 nm), and Thr342 (around 0.2 nm). Overall, both results are highly consistent with the docking study results illustrated in Fig. 4.
Structural dynamics calculated during the 100 ns of MD trajectories; Root Mean Square fluctuation (RMSF) of hIDO1 protein backbone (A), number of H-bonds formed with hIDO1 native ligand (B) and with Pitavastatin (C).
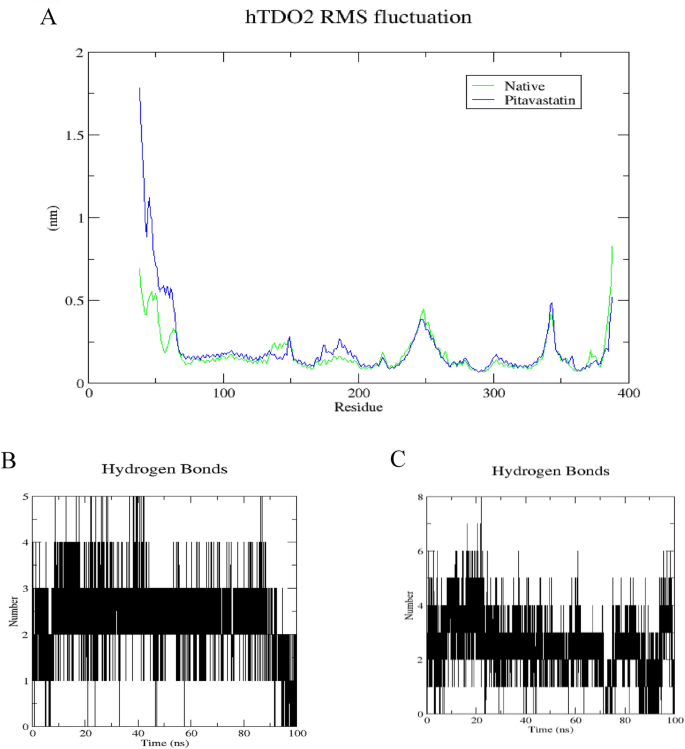
Structural dynamics calculated during the 100 ns of MD trajectories; Root Mean Square fluctuation (RMSF) of hTDO2 protein backbone (A), number of H-bonds formed with hTDO2 native ligand (B) and with Pitavastatin (C).
To further elucidate the stability of these interactions, the number of hydrogen bonds formed during the 100 ns simulation was quantified (refer to Figs. 6B, C, 7B, and C). In the case of hIDO1, the co-crystallized ligand maintained 1â2 hydrogen bonds during the initial 75 ns of the simulation, whereas Pitavastatin demonstrated a larger number of stable hydrogen bonds (2â3) throughout the entire simulation, with occasional formation of a third and fourth bond in certain frames. Similarly, for hTDO2, an average of 2â4 hydrogen bonds was observed throughout the trajectory, correlating with the high stability observed in both RMSD and Rg plots. Pitavastatin also exhibited the ability to form stable 2â4 hydrogen bonds over the entire 100 ns simulation duration.
These findings underscore the favorable binding affinity of Pitavastatin and the co-crystallized ligands to their respective target receptors, highlighting the importance of stable hydrogen bond formation in driving robust ligand-receptor interactions.
In vitro hIDO1 and hTDO Inhibitor Screening Assay
Two in vitro enzymatic inhibition assays were selected to assess Pitavastatin inhibition activity against hIDO1 and hTDO2 enzymes and compare this inhibition activity to that of the positive control. IC50 values listed in Table 4 and Fig. 8 confirm the previous findings of the docking study where Pitavastatin showed an inhibition activity against both enzymes in nM (351 and 588 nM for hIDO1 and hTDO2, respectively) confirming its dual inhibition activity being more potent towards hIDO1.
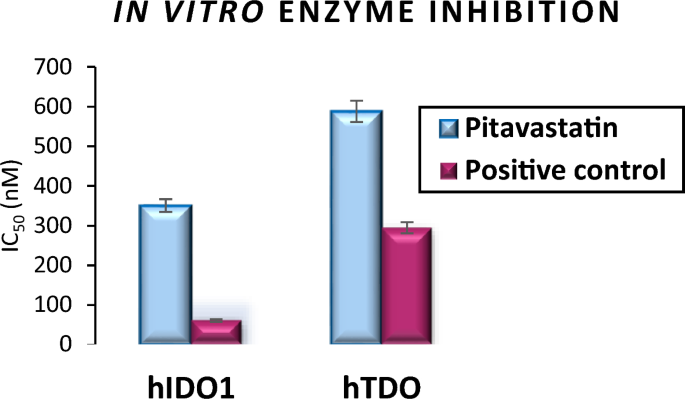
A graphical representation for Pitavastatin inhibition activity against hIDO1 and hTDO2 enzymes compared to the positive control, represented in IC50 (nM).
MTT cytotoxicity assay
As shown in Table 5 and Fig. 9, Pitavastatin demonstrated a potent cytotoxic effect on all three tested cancer cell lines BT-549, MCF-7, and HepG2, respectively. However, the highest response was that of the liver cancer HepG2 cell lines which were almost 9.14-fold more sensitive than BT-549 and 5.17-fold more responsive than MCF-7 to Pitavastatin treatment.
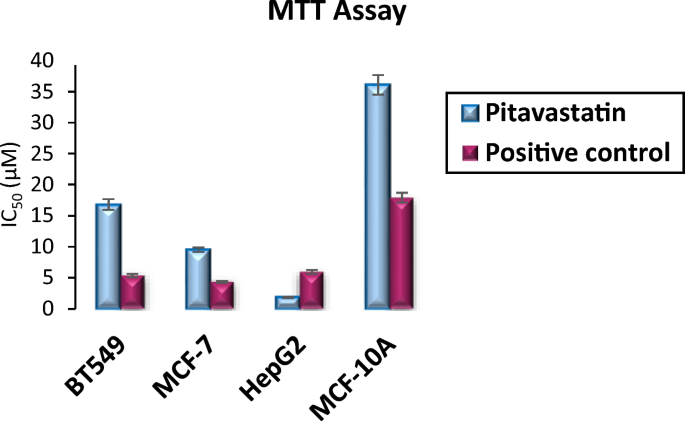
A graphical representation of cellular IC50 of Pitavastatin compared to control against BT-549, MCF-7, HepG2 and MCF-10A cell lines.
Additionally, Pitavastatin showed to be highly selective affecting higher cytotoxicity to cancer cell lines BT-549, MCF-7, and HepG2 in contrast to its lower toxic effect on the normal cell line MCF-10A with IC50 values of 16.82, 9.52, 1.84, and 36.07 µM, respectively. Pitavastatin is 2.14-fold selective to BT-549 over MCF-10A, 3.79-fold selective to MCF-7, and 19.6-fold selective to HepG2 cells. Conclusively, Pitavastatin demonstrated a high safety margin and selective cytotoxicity towards different cancer cell lines with little cytotoxicity towards the tested normal cell line.
The mechanism underlying Pitavastatin’s dual inhibitory action on hIDO1/hTDO2 is of particular interest. By targeting multiple nodes within Trp catabolic pathway, Pitavastatin may offer a more effective and comprehensive approach to disease management. hIDO1 and hTDO2 play key roles in tryptophan metabolism, which is implicated in immune regulation and tumor immune escape. By inhibiting both enzymes, Pitavastatin could disrupt Trp metabolism in cancer cells, potentially altering the tumor microenvironment and enhancing immune surveillance against cancer cells26. This dual inhibition may contribute to Pitavastatin’s anticancer activity observed across different types of cancer.
Statins have been reported to have an anticancer effect due to their antioxidant, anti-inflammatory and antiproliferative activities against various types of cancer cells like ovarian, breast, prostate, colon, lung, brain, cancers, and melanoma27. They were also found to have a synergetic effect when combined with other chemotherapies like doxorubicin, topotecan and paclitaxel28. In addition to their anticancer effect, patients using statins reported low risks for cancer development as high cholesterol levels are correlated with cancer development29. Furthermore, Pun et al.30 reported the apoptotic activity (autophagy-mediated) of Pitavastatin upon treatment in oral squamous cell carcinoma cells (SCC15) and colon cancer cells (SW480).
To contextualize its efficacy and compare it to existing inhibitors, we can examine previous studies and clinical trials on both single-target and dual inhibitors of hIDO1 and hTDO2. Single-target inhibitors of hIDO1 and hTDO2, such as epacadostat (hIDO1 inhibitor) and navoximod (hTDO2 inhibitor), have been investigated extensively in preclinical and clinical settings. For example, epacadostat was evaluated in combination with immune checkpoint inhibitors in various solid tumors, including melanoma and lung cancer. Despite promising preclinical data suggesting synergy between hIDO1 inhibition and immune checkpoint blockade, clinical trials failed to demonstrate significant improvements in overall survival or progression-free survival compared to standard of care treatments31,32,33. Similarly, navoximod showed limited efficacy as a single agent in early-phase clinical trials, prompting further exploration of combination strategies32.
In contrast, dual inhibitors of hIDO1 and hTDO2 offer a unique advantage by targeting two key enzymes involved in tryptophan metabolism within the tumor microenvironment. Preclinical studies have shown that simultaneous inhibition of hIDO1 and hTDO2 may lead to more pronounced anticancer effects compared to single-target inhibitors. For example, a recent study by Li et al.34 demonstrated that dual inhibition of hIDO1 and hTDO2 using a small molecule inhibitor resulted in enhanced antitumor immune responses and tumor regression in mouse models of melanoma and colon cancer. This suggests that targeting both enzymes simultaneously may overcome potential compensatory mechanisms and improve therapeutic outcomes.
Flow cytometry apoptosis assay and cell cycle analysis
Since MTT cytotoxicity assay unveiled the significant cytotoxic effect of Pitavastatin on the three tested cancer cell lines, further evaluation was needed to investigate the mechanism of cell death. HepG2 was selected for all further in vitro mechanistic investigations as it was the most affected cancer cell line when treated with Pitavastatin (showing very low IC50 valueâ=â1.84 µM).
Apoptotic and necrotic cell population percentage was determined for HepG2 cell line after 48 h of treatment with the pre-calculated IC50 values of Pitavastatin via annexin-FITC/propidium iodide (AV/PI). Cell apoptosis assay results on HepG2 cells (Fig. 10) demonstrate the percentage of live cells decreased from 97.88% (control) to 56.83% when treated with Pitavastatin. Total cell death is reported to be 43.17%, whereas the sub-populating in early apoptosis increased to 23.27%, the average late apoptotic sub-population count reached 15.94% and an increase in necrosis was also observed (about 2.5 times more than control untreated cells). The results proved that the Pitavastatin effectively induced apoptosis, substantially early apoptosis followed by late apoptosis, in HepG2 cells. Similar results were obtained by Abdullah et al.35 reporting significant early or late apoptosis when Pitavastatin was applied in combination with Prednisolone on ovarian cancer cell lines (Ovcar-4 and Cov-362). Likely, late apoptotic/necrotic phase cell death was observed as a result of the synergetic combination of Pitavastatin and Gemcitabine on human MIA PaCa-2 cell line (pancreatic carcinoma)36. Also, late apoptosis was observed upon incubating preactivated T-cells with high concentration of Pitavastatin as a result of caspase-3/7 activation37.
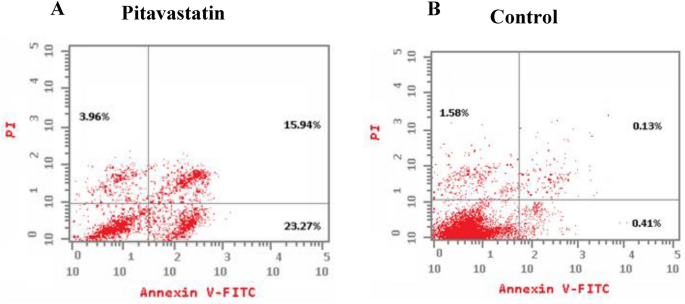
Induction of apoptosis in HepG2 cells by annexin-V/propidium iodide stain. Cytograms showing HepG2 cells treated with Pitavastatin (1.84 µM, 48 h) (A), HepG2 cells as an untreated control (B).
Afterwards, a cell cycle analysis test was utilized to study the cell proliferation percentage in different cell cycle phases. The highest cell arrest induction was observed in G1 and S phases with 1.11-fold and 1.14-fold, respectively (52.61% and 44.01%, respectively) when compared to the control as shown in Fig. 11. These results affirm that Pitavastatin induces G1/S phase arrest in HepG2 cancer cell line. Pitavastatin was also reported to induce S-phase cell cycle arrest in human U937 monocytic tumor cells38. Additionally, cell apoptosis via G1 cell cycle arrest was noticed during combined Pitavastatin- dacarbazine treatment39.
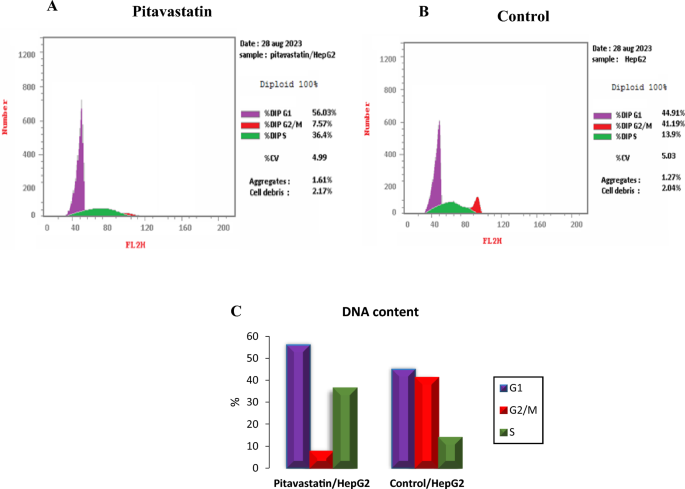
Cell cycle analysis cytograms of Pitavastatin-treated HepG2 cells (A), control untreated HepG2 cells (B) and percentage of HepG2 cell population in various cell cycle phases (C).
ELISA assay and RT-PCR for cell cycle regulators
The expression levels of hIDO1, hTDO2, STAT3, P21, P27, IL-6, AhR and Caspase3 as cell cycle regulators and markers of cell cycle arrest were measured using ELISA Kit to demonstrate the mechanism by which Pitavastatin inhibits HepG2 cells survival. As shown in Table 6 and Fig. 12, treatment with Pitavastatin has affected significant downregulation of the expression of both hIDO1 and hTDO2 by 2.9- and 2.7-fold, respectively, thus, affirming the dual hIDO1/hTDO2 inhibition capability of Pitavastatin.
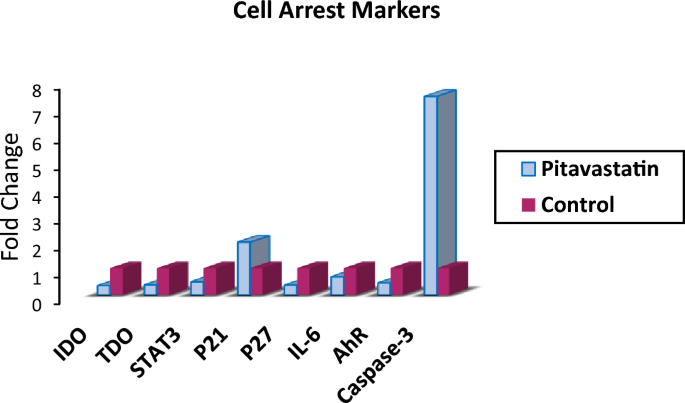
A graphical representation of different Cell arrest markers expression upon Pitavastatin treatment on HepG2 cells.
Previous studies reported that high hIDO1 levels in various cancer cells are induced by IL-6 and others reported that hIDO1 can activate and upregulate IL-6 at the early stage of tumorigenesis to influence inflammatory conditions and facilitate cancer growth40. Also, the inhibition of IL-6 using siRNA and/or pharmacological inhibitors was found to reduce IDO mRNA and protein expression as well as kynurenine formation41. Accordingly, IL-6 expression is a critical biomarker to evaluate and confirm the anticancer capability of Pitavastatin against HepG2. Indeed, treating HepG2 cells with the predetermined IC50 value has resulted in lowering the level of IL-6 (91.83Â pg/mL) compared to control untreated cells (135.3Â pg/mL).
The effects of the IDO-AHR-IL-6-STAT3 loop in HepG2 were also evaluated. Previous research suggests that targeting the IDO-AHR-IL-6-STAT3 loop may reverse immune suppression caused by IDO142,43,44,45. Sustained hIDO1 expression requires constitutively active STAT3, which is regulated by autocrine IL-6 through phosphorylation and acetylation46. Our findings indicate a decrease of approximately 50% in STAT3 and 55% in AhR, confirming Pitavastatinâs effective therapeutic intervention with the immune suppression loop. AhR downregulation is essential, as activation of AhR may result in pro-cancerous effects in several human malignancies and may have a role in poor prognosis.47,48. Additionally, some studies have shown that cancer cells that overexpress hTDO2 and activate AhR are able to evade immune surveillance49.
The pro-apoptotic effect of inhibiting hIDO1 and hTDO2 is correlated with p21 and p27 inhibition. hIDO1/AhR pathway deactivation was found to downregulate the cell cycle inhibitor p27 which induces G1/S phase blockage50,51. In our study a 63.78% reduction in p27 expression was observed for Pitavastatin treated HepG2 cells compared to the control untreated cells as shown in Fig. 12. On the other hand, p21 expression increased 2 times more than the control, however, hIDO1 inhibition was previously reported to decrease p21 expression in T cells which in turn leads to apoptosis52. This abnormal overexpression of p21 in HepG2 after Pitavastatin treatment was also previously reported in human U937 monocytic tumor cells treated with Pitavastatin38,39. It remains unknown whether this high p21 level affects cancer progression so further investigation is needed.
Elevated levels of caspase-3 are widely recognized to induce cellular apoptosis by cleaving various downstream substrates, resulting in characteristic morphological changes that serve as a significant marker of apoptosis53. In this study, caspase-3 level increase 7.4-fold upon Pitavastatin treatment compared to the control untreated cells.